Liver cirrhosis is a chronic, progressive condition that affects the liver, leading to scarring and liver dysfunction. Understanding the stages of liver cirrhosis is crucial for early detection, effective management, and improving patient outcomes. This blog will delve into the different stages of liver cirrhosis, their symptoms, causes, and available treatment options.
What is Liver Cirrhosis?
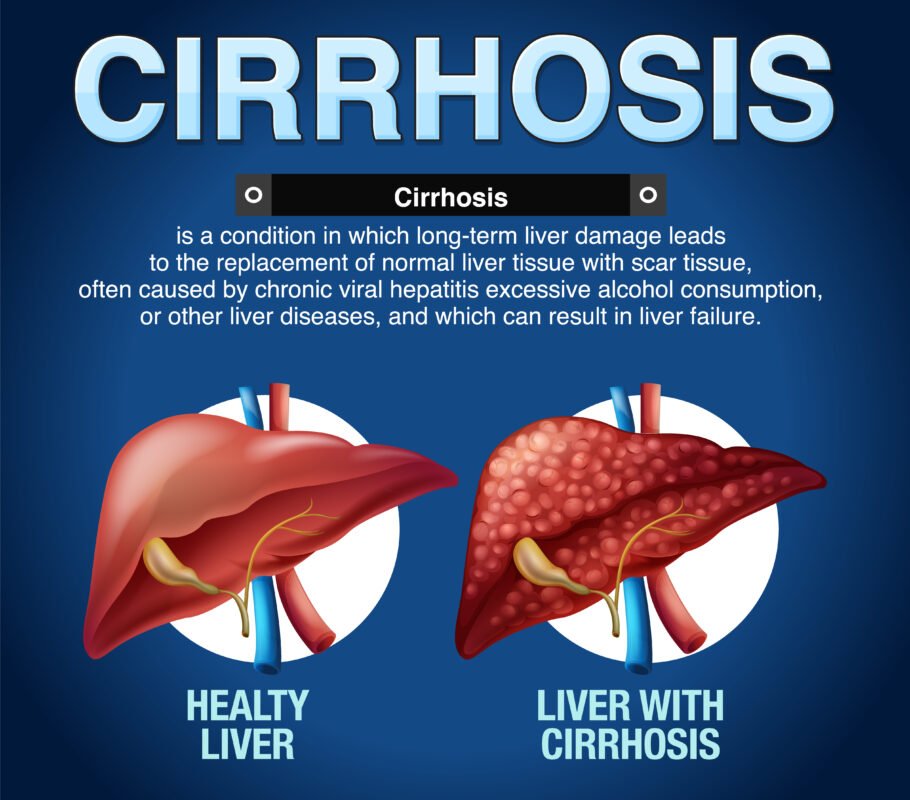
Cirrhosis is the result of long-term, continuous damage to the liver and may be due to many different causes. When the liver is injured, it tries to repair itself, leading to the formation of scar tissue. Over time, more and more scar tissue forms, making it difficult for the liver to function properly. Advanced cirrhosis is life-threatening, highlighting the importance of early diagnosis and intervention.
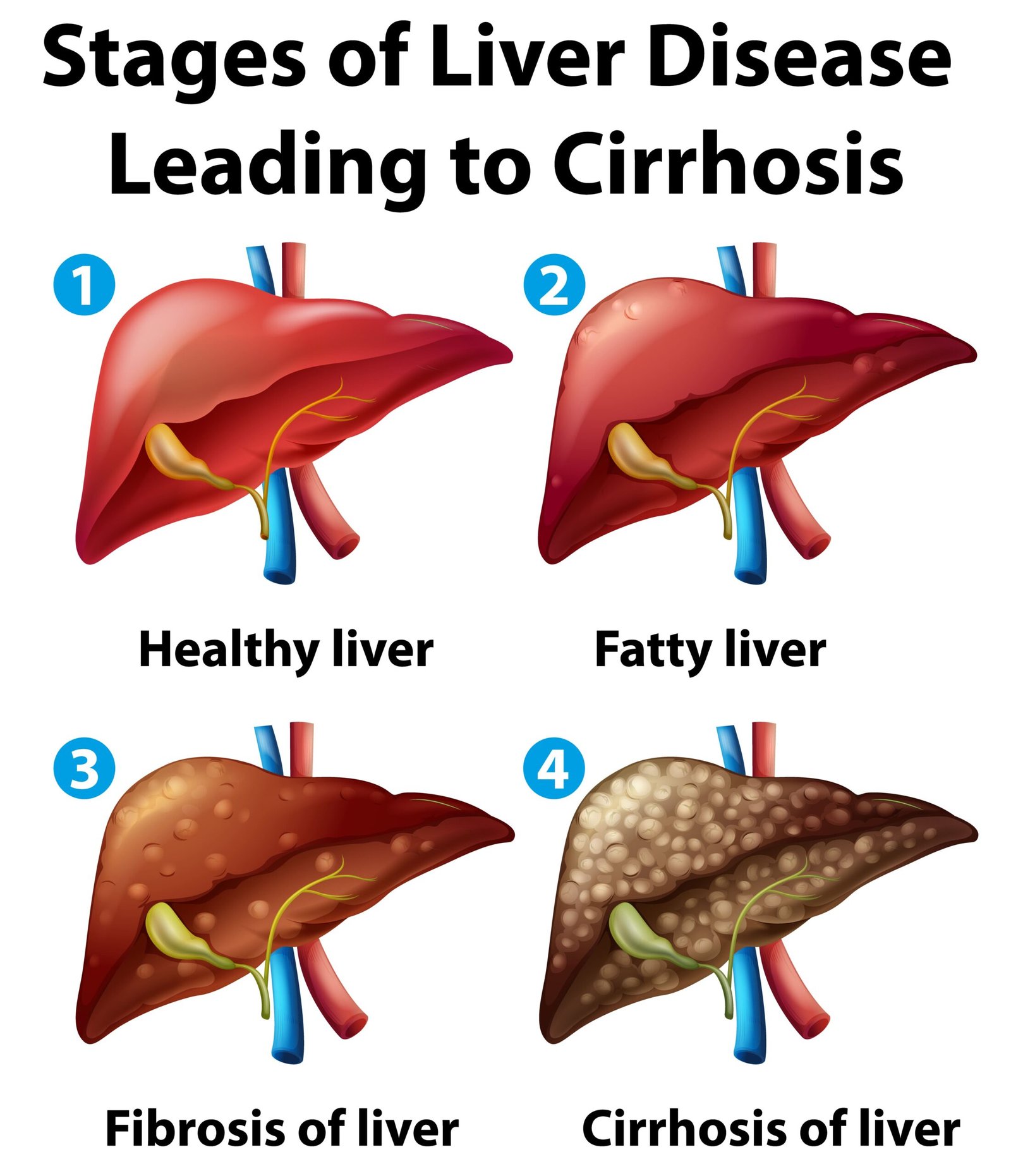
Stages of Liver Cirrhosis
Liver cirrhosis progresses through four main stages, each with distinct characteristics and implications for health.
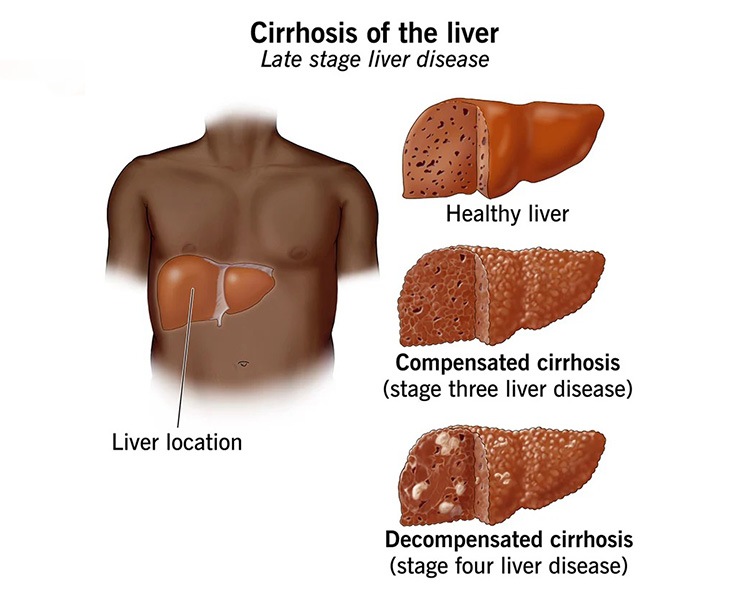
Stage 1: Compensated Cirrhosis
In the initial stage, known as compensated cirrhosis, the liver still functions relatively well despite some scarring. Many individuals at this stage experience no symptoms, making it challenging to detect without medical testing. Some possible signs include mild fatigue, weakness, and occasional abdominal discomfort.
Diagnosis and Management:
- Diagnosis: Blood tests, imaging studies (ultrasound, CT scan), and sometimes liver biopsy are used to diagnose cirrhosis.
- Management: Focus on treating the underlying cause (e.g., antiviral medications for hepatitis, lifestyle changes for alcohol-related cirrhosis). Regular monitoring and a healthy lifestyle can help slow the progression.
Stage 2: Compensated Cirrhosis with Varices
As cirrhosis progresses to the second stage, more noticeable symptoms may emerge due to increased pressure in the portal vein (portal hypertension). This can lead to the development of varices (enlarged blood vessels) in the esophagus and stomach, which can bleed easily.
Symptoms:
- Swollen veins (varices) that can bleed
- Increased fatigue
- Mild to moderate abdominal swelling
Diagnosis and Management:
- Diagnosis: Endoscopy can detect varices. Routine blood tests and imaging continue to monitor liver function.
- Management: Beta-blockers to reduce portal hypertension, banding of varices, and continued treatment of the underlying cause. Avoiding alcohol and managing diet are critical.
Stage 3: Decompensated Cirrhosis
In decompensated cirrhosis, the liver is significantly scarred and unable to perform essential functions effectively. This stage is characterized by severe symptoms and complications that can significantly affect quality of life.
Symptoms:
- Jaundice (yellowing of the skin and eyes)
- Significant abdominal swelling (ascites)
- Confusion and memory problems (hepatic encephalopathy)
- Severe fatigue and muscle wasting
- Frequent infections
Diagnosis and Management:
- Diagnosis: Comprehensive liver function tests, imaging, and frequent monitoring.
- Management: Diuretics for ascites, lactulose for hepatic encephalopathy, antibiotics for infections, and potential liver transplantation evaluation. Intensive medical support and lifestyle modifications are crucial.
Stage 4: End-Stage Liver Disease (ESLD)
End-stage liver disease is the final stage of cirrhosis where the liver function is severely compromised. Patients at this stage often face life-threatening complications and require immediate medical intervention.
Symptoms:
- Persistent jaundice
- Severe ascites and edema
- Increased risk of liver cancer
- Persistent hepatic encephalopathy
- Renal (kidney) failure
Diagnosis and Management:
- Diagnosis: Advanced imaging, liver biopsy, and frequent blood tests to monitor organ function.
- Management: Liver transplantation is often the only definitive treatment. Supportive care includes managing symptoms, frequent hospitalizations, and end-of-life care planning.
Causes of Liver Cirrhosis
Several factors can contribute to the development of liver cirrhosis, including:
- Chronic Alcohol Abuse: Long-term alcohol consumption is a leading cause.
- Chronic Viral Hepatitis: Hepatitis B and C infections.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Associated with obesity and metabolic syndrome.
- Autoimmune Liver Diseases: Such as autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis.
- Genetic Disorders: Hemochromatosis, Wilson’s disease.
- Chronic Bile Duct Diseases: Such as bile duct cancer or strictures.
Prevention and Early Detection
Preventing liver cirrhosis involves addressing its root causes:
- Limiting alcohol intake
- Maintaining a healthy weight
- Managing chronic medical conditions
- Getting vaccinated for hepatitis B
- Regular medical check-ups for those at risk
Conclusion
Understanding the stages of liver cirrhosis is vital for early detection and effective management. While the condition can progress silently in its early stages, timely intervention can significantly improve outcomes and quality of life. By addressing the underlying causes and adhering to medical advice, individuals can manage their condition and potentially prevent the progression to more severe stages. Regular medical follow-ups and a proactive approach to liver health are key to combating this chronic liver disease.